UR School of Nursing Celebrates Nurse Practitioner Week
By Jessica O'Leary
Monday, November 14, 2016

Fifty years ago in 1966, the UR School of Nursing created its first nurse practitioner program, one year after Dr. Loretta “Lee” Ford co-developed the nurse practitioner model and started the nation’s first NP program in Colorado.
In the past five decades, the nurse practitioner model has flourished at the University of Rochester, thanks to the school’s progressive approach and its collaboration with the Medical Center. Graduates of the program have gone on to become leaders and educators, helping to ensure access to care for vulnerable populations, prevent disease, promote health, manage chronic illnesses, and improve end-of-life care. And, more than ever, they are at the table when key health care decisions are being made.
In celebration of Nurse Practitioner Week, held Nov. 13-19, three UR School of Nursing graduates and students shared their stories about what motivated them to become a nurse practitioner and how they hope to serve their communities and their patients.
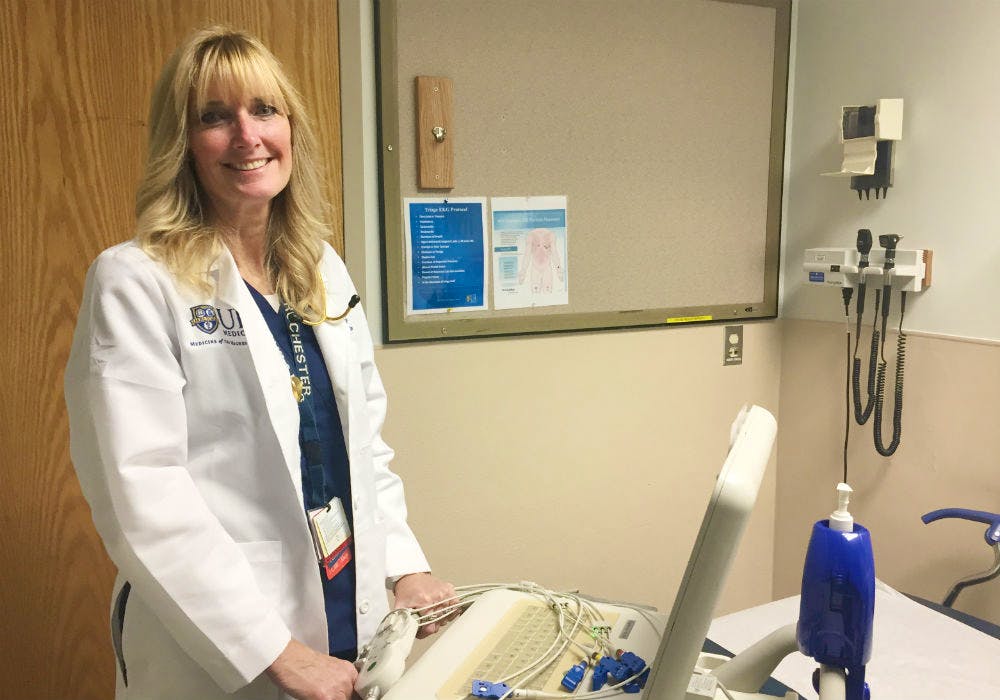
Dolores “Dee” Krebs, MS, APRN, BC, FNP, SANE-A, SANE-P, NYSafe, FAANP
Family nurse practitioner in the University of Rochester Medical Center Emergency Department
Although Dee Krebs has worked at the Medical Center for 33 years and has been a nurse on nearly every floor of the hospital, it’s easy for her to pick her favorite job.
“I really love working in the emergency room. It can be chaotic, and it’s not for everyone, but it keeps me on my toes and it’s very rewarding,” she said. “I enjoy putting the pieces of the puzzle together, figuring out what might be wrong, and playing a role in their treatment plan.”
Krebs, who became a nurse practitioner 18 years ago, has helped make an impact on the lives of some of the most vulnerable patients who come into the emergency department — victims of violence and sexual assault. She helped establish UR Medicine’s Sexual Assault Nurse Examiner (SANE) program, which provides training for health care providers who care for victims of abuse.
“Before the program was in place, there really was a lack of training — not just here, but across the state,” said Krebs. “Nurses were told to collect a crime kit, but they didn’t know why or how to work with the patient or coordinate with law enforcement. Victims often waited for hours before being seen, because there wasn’t any special protocol for them. As a result, things fell through the cracks.”
Krebs now provides training for nurse examiners, who become skilled in managing patients’ medical forensic exams, providing emotional and social support, and providing testimony in court.
“I also work closely with law enforcement and help educate first responders,” said Krebs. “Working together ensures that we are giving these patients top-notch medical forensic care and that if the patient chooses to move forward with criminal charges, we’re doing everything we can for them.“
Although Krebs is likely busy enough as it is, she’s also been an active legislative advocate for nurse practitioners, she precepts UR School of Nursing students, she helped found the local chapter of the New York State Nurse Practitioner Association, and she’s the president of the International Association of Forensics.
But despite her many accomplishments and the awards she’s won, she says one of the most rewarding parts of her job is when she’s able to testify in court and help a victim she cared for in the hospital.
“The work can be tough, and it can have an impact on us as nurses,” said Krebs. “But when I’m able to testify and we have a favorable outcome, I know that all the work I’m doing is worth it.”
Julie Apperson, RN
Student in the psychiatric mental health nurse practitioner program
As a high school and college student, Julie Apperson wasn’t sure what career path she wanted to take. Although her mother was a nurse, she had never seriously thought about a career in the field.
“I took the most random selection of courses you could choose in my first semester of college,” she said. “I remember sitting down with my father, and he said, ‘You would be the most awesome nurse.’ My father gave me the greatest gift that day.”
After that heart-to-heart, Apperson set her sights on a career in nursing. She’s now been in the field for nearly three decades, and for the past 10 years, she has worked in Chautauqua County government as an RN case manager, RN supervisor, and program director for the Chautauqua County Opioid Overdose Program.
“I feel like I’ve gotten more back from being a nurse than I’ve ever put into it,” she said. “It’s a natural antidepressant, and when you are able to help people through your work, it has such a therapeutic effect.”
Over the years, Apperson developed a personal interest in caring for individuals who have both a substance abuse disorder and a mental health disorder.
“My work and my own personal experience with a family member who was struggling with substance misuse steered me in that direction,” she said. “The system is extremely disjointed and patients are stigmatized, and I really wanted to be part of a movement of change.”
To play a role in that movement, Apperson sought out a nurse practitioner program focused on psychiatric mental health. Despite living more than two hours away from Rochester, she chose the UR School of Nursing program because she believed it offered a comprehensive education that would give her the preparation she needed to make a considerable career shift. After graduating in December, she hopes to specialize in addiction medicine.
On top of work, school, and family obligations, Apperson has gone the extra mile to be an advocate for issues surrounding substance abuse. She’s an active volunteer with Families for Sensible Drug Policy, and she has implemented a training program for county jail inmates that teaches them how to be overdose responders.
“It’s a perfect opportunity for intervention, and from a public health standpoint, it’s been a missed opportunity,” said Apperson. “It’s programs like this one that I think can make a difference in our communities.”
Luke Angell, MS, RN, PPCNP-BC
Pediatric nurse practitioner at Golisano Children’s Hospital
Luke Angell hasn’t taken a break from school since kindergarten. After receiving his bachelor’s degree from Cornell University, he enrolled in the UR School of Nursing’s accelerated program. Immediately after graduating as a nurse, he set his sights on becoming a nurse practitioner.
Now, he’s working toward a doctoral degree — an accomplishment he hopes to check off his list in 2018.
“I can finally see the light at the end of the tunnel,” he joked.
Angell’s consistent motivation to advance his career stems from his own personal experience. Twenty-six years ago, he was born prematurely — three months early — weighing just 2 ½ pounds.
“I always knew I wanted to be in health care because I spent so much time with doctors, nurses, and physical therapists growing up,” he said. “I wanted to be able to give back to all the people who helped me.”
Although Angell was sure he wanted to help care for young patients, for years, he wasn’t sure if wanted to pursue nursing school or medical school – until he heard about the UR School of Nursing and immediately knew it was the perfect fit.
“I fell in love with the school because of its robust clinical and research programs,” said Angell. “The clinically based faculty were really able to make things come to life by translating what we were learning in the classroom into clinical practice.”
Angell has now been a nurse for four years, and he’s already served in several different roles. He’s been a pediatric staff nurse, a teacher in the school’s accelerated program, and he’s worked in a pediatric-pulmonary clinic.
“I find my job rewarding because kids are so resilient, and I consider it a real privilege to have an impact on their lives,” said Angell. “I have rocked a crying newborn in the wee hours of the morning to soothe them back to sleep, I have reassured a toddler as they woke up from a recent surgical procedure, I have given a high five to a school-aged patient as he headed out the door after spending weeks in the hospital, I have shared encouraging words with an adolescent who was recovering from a recent orthopaedic injury, and I have lent a listening ear to a family in their time of need.”
Now, Luke is a pediatric advanced practice nurse educator in an inpatient unit at Golisano Children’s Hospital, where he says he’s able to have more of a “big-picture” approach and help develop policies and guidelines to help improve patient care and educate staff.
Although he’s always been thinking about the next step in his career, for now, Angell said he’s happy to be where he is and to focus on earning his Doctor of Nursing Practice degree.
“I am confident that the UR School of Nursing has given me the skills to succeed in caring for children in their time of need, whether it be through teaching the next generation of nurses, lobbying for health care policies that impact the lives of children, leading a pediatric health care team, or researching and translating the most up-to-date clinical evidence into practice,” said Angell.