Creating Safe Spaces: Simulation Training Helps Future NPs Discuss Sexual Health with Empathy, Skill
By Sandra Parker
Friday, January 3, 2025
Gathering information from patients about their sexual health is crucial to overall wellness, yet evidence shows that clinicians need practice getting comfortable broaching the topic. A new School of Nursing study is addressing this gap in education by providing a realistic opportunity for new nurse practitioners to develop the skills needed to put the patient at ease enough to fully discuss the topic.
“We’re always looking at innovative ways to make the education we provide more meaningful and to make a lasting impression,” said School of Nursing research scientist Natalie Leblanc, PhD, MPH, RN. “Sexual behavior is still very stigmatizing and tends to incur judgment, and sometimes that’s on the part of the provider.”
A comfortable and skillful clinician can more easily gain the patient’s trust and draw out information needed for advising on preventative measures and treatment services and, ultimately, improving patient outcomes and stopping the spread of viruses.
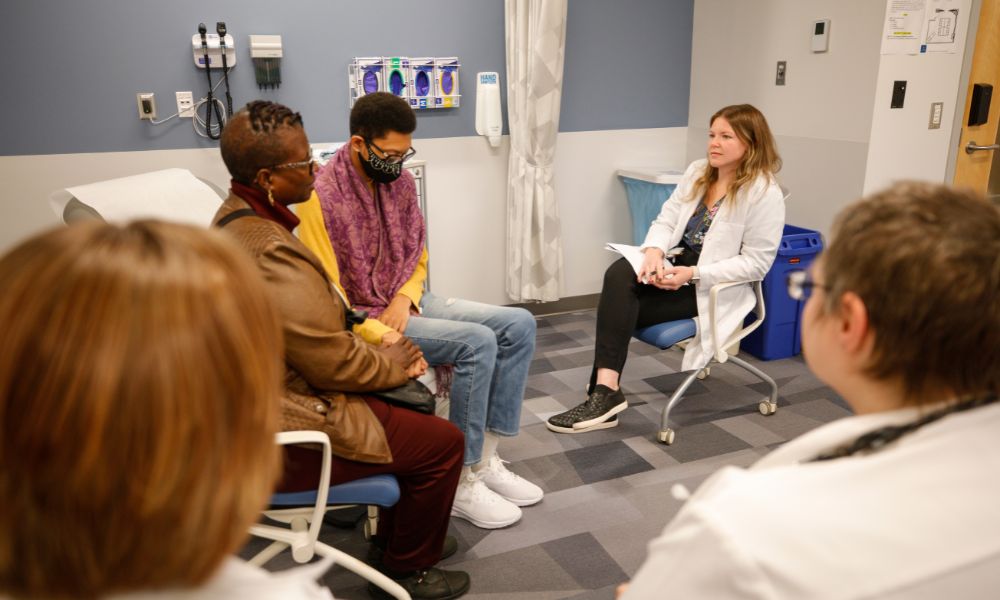
“We don’t need to shy away from taking a patient’s history,” said Erin Baylor, DNP, RN, PCPNP-BC, ONP, CHSE, director of simulation and specialty director for the Pediatric Nurse Practitioner program. “There’s a skill involved to create a nonjudgmental conversation with our clients and their family members that fosters an honest dialogue.”
Nationally, the rate of sexually transmitted infections (STIs) remains high with more than 2.5 million new infections each year, according to the Centers for Disease Control and Prevention. Left untreated, STIs can lead to certain cancers and infertility. Rates of syphilis and congenital syphilis are rising at an alarming rate; CDC data from 2022 shows a 74 percent increase over the past five years.

Leblanc and Baylor recently finished the simulation portion of their study, which used trained standardized patients to “replicate what we knew were the challenges existing in clinical practice. It was an authentic encounter and a psychologically safe space for students to be autonomous in decision making,” Leblanc said.
Simulations focused on three types of encounters: visits with the patient alone, with the patient and a partner, and with an adolescent and a parent. Topics included gender dysphoria, HPV vaccination, sexual dysfunction, pre- and post-exposure to STIs, couple-centered care, HIV status neutral approaches, and HIV prevention and care. Skills to be developed included “best practices in patient engagement, use of anti-stigmatizing language, emphasis on reasons instead of risks in communication with patients, and comprehensive sexual health history taking.”
So far, results point to the study as a success.
“One student said that in clinical rotations, they may be asked to step aside when there is a high-stakes situation,” Leblanc said. “The simulation allowed them to be part of what they’re missing.”
Baylor noted that nurse practitioner students – along with nurses, doctors, and other advanced practice providers from the medical center who were involved with the training – referred to it as “a gift.”
| Say this: | Not this: |
|---|---|
| People living with HIV | HIV-infected (can imply a contagious or threatening condition) |
| Sexual orientation | Sexual preference (to avoid suggesting a choice) |
| Multiple sexual partners | Promiscuous (to avoid judgement) |
| Survivor (to highlight strength) | Victim |
| Disproportionately affected (to acknowledge the broader social factors at play) | Vulnerable or at-risk |
As part of the study, Baylor, Leblanc and other instructors planned to debrief with students and review videos of the student interactions.
Next semester, focus groups will be conducted with student learners to determine which parts of the simulation worked well and which parts need to be amended. Leblanc and Baylor believe that the results will justify retaining the simulations as part of the standard training curriculum at the School of Nursing.
The study was funded by the Drs. Jeremy A. Klainer and Pamela York Klainer Endowed Award at the School of Nursing, which supports efforts to further the School’s strategic priorities. As collaborators on the project, Leblanc and Baylor believe it serves as a model of collaboration between research and education missions, integrating innovative nursing simulation with research aimed at promoting sexual health and wellness.
Categories: Nurse Practitioner Programs, Master's Programs, Research

